- English
- French
- German
- Portuguese
- Spanish
- Russian
- Japanese
- Korean
- Arabic
- Greek
- German
- Turkish
- Italian
- Danish
- Romanian
- Indonesian
- Czech
- Afrikaans
- Swedish
- Polish
- Basque
- Catalan
- Esperanto
- Hindi
- Lao
- Albanian
- Amharic
- Armenian
- Azerbaijani
- Belarusian
- Bengali
- Bosnian
- Bulgarian
- Cebuano
- Chichewa
- Corsican
- Croatian
- Dutch
- Estonian
- Filipino
- Finnish
- Frisian
- Galician
- Georgian
- Gujarati
- Haitian
- Hausa
- Hawaiian
- Hebrew
- Hmong
- Hungarian
- Icelandic
- Igbo
- Javanese
- Kannada
- Kazakh
- Khmer
- Kurdish
- Kyrgyz
- Latin
- Latvian
- Lithuanian
- Luxembou..
- Macedonian
- Malagasy
- Malay
- Malayalam
- Maltese
- Maori
- Marathi
- Mongolian
- Burmese
- Nepali
- Norwegian
- Pashto
- Persian
- Punjabi
- Serbian
- Sesotho
- Sinhala
- Slovak
- Slovenian
- Somali
- Samoan
- Scots Gaelic
- Shona
- Sindhi
- Sundanese
- Swahili
- Tajik
- Tamil
- Telugu
- Thai
- Ukrainian
- Urdu
- Uzbek
- Vietnamese
- Welsh
- Xhosa
- Yiddish
- Yoruba
- Zulu
Is Pure D-alpha Tocopherol Effective in Treating Vitamin E Deficiency?
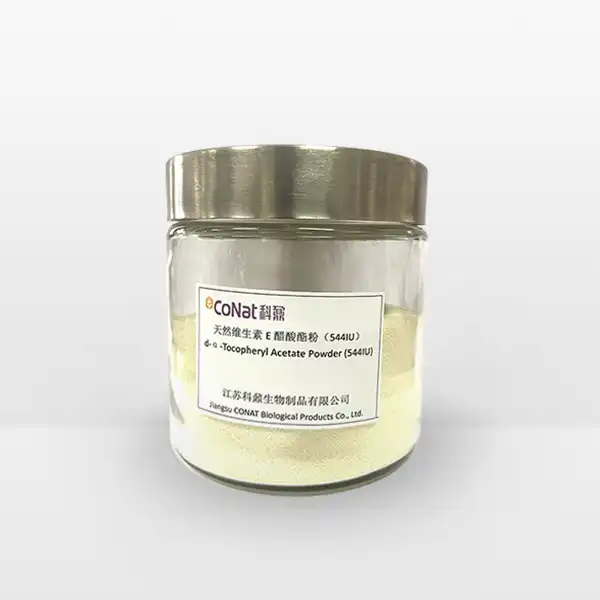
Vitamin E deficiency is a significant nutritional concern that can lead to various health complications if left untreated. Among the different forms of vitamin E supplements available, pure D-alpha tocopherol has emerged as a prominent treatment option. This natural form of vitamin E is particularly interesting due to its high bioavailability and potent antioxidant properties. Understanding its effectiveness in treating vitamin E deficiency is crucial for healthcare providers and patients alike, as proper supplementation can prevent and reverse deficiency-related symptoms. Recent clinical studies have demonstrated that pure D-alpha tocopherol supplementation can effectively address both acute and chronic deficiency states, with particularly promising results in patients with malabsorption disorders. The compound's role in preventing oxidative stress-related damage has garnered increased attention, especially in conditions where cellular membrane integrity is compromised. Furthermore, emerging research suggests that D-alpha tocopherol may have broader therapeutic applications beyond simple deficiency treatment, including potential neuroprotective effects and benefits for cardiovascular health.
What Makes D-alpha Tocopherol Different from Other Forms of Vitamin E?
D-alpha tocopherol stands out among vitamin E compounds due to its unique molecular structure and biological activity. This natural form of vitamin E is the most bioactive and readily absorbed by the human body compared to other tocopherol variants. The 'D' prefix indicates its natural origin, distinguishing it from synthetic forms that typically carry the 'DL' prefix. The molecular structure of D-alpha tocopherol perfectly matches the body's vitamin E receptors, allowing for optimal absorption and utilization.
When comparing D-alpha tocopherol to other vitamin E forms, several key factors demonstrate its superiority. First, its absorption rate is significantly higher than synthetic alternatives, with studies showing up to 50% better absorption compared to synthetic DL-alpha tocopherol. The body preferentially retains D-alpha tocopherol in tissues and organs, while other forms are more quickly eliminated. This natural form also demonstrates enhanced antioxidant activity, providing better protection against free radical damage at the cellular level.
Research has shown that Pure D-alpha Tocopherol's effectiveness stems from its ability to maintain cell membrane integrity, support immune function, and protect against oxidative stress. Its molecular configuration allows it to interact more effectively with cell membranes, ensuring better distribution throughout the body's tissues. This form of vitamin E also shows superior ability to cross the blood-brain barrier, making it particularly valuable for neurological health.
Recent molecular studies have unveiled additional mechanisms behind D-alpha tocopherol's enhanced efficacy. The compound's stereochemistry plays a crucial role in its interaction with cellular transport proteins, particularly α-tocopherol transfer protein (α-TTP). This protein specifically recognizes and preferentially binds to the natural D-alpha form, facilitating its incorporation into very-low-density lipoproteins (VLDL) for systemic distribution. The stereospecific binding also influences the compound's half-life in tissues, with D-alpha tocopherol showing significantly longer retention times compared to synthetic alternatives.
Furthermore, D-alpha tocopherol's superior antioxidant capacity extends beyond direct free radical scavenging. Research has revealed its involvement in cell signaling pathways, particularly those related to inflammation and immune response modulation. The compound has been shown to regulate the expression of genes involved in cellular stress response, potentially explaining its broader therapeutic benefits. Its ability to maintain membrane fluidity and structure also contributes to cellular homeostasis, particularly in tissues with high metabolic activity.
How Much D-alpha Tocopherol Should Be Taken Daily for Optimal Results?
Determining the optimal dosage of Pure D-alpha Tocopherol requires careful consideration of several factors, including age, health status, and the severity of deficiency. The Recommended Dietary Allowance (RDA) for vitamin E in adults is 15 mg (22.4 IU) of alpha-tocopherol per day. However, therapeutic doses for treating deficiency often differ from these maintenance levels.
For mild to moderate vitamin E deficiency, healthcare providers typically recommend doses ranging from 100 to 400 IU daily. These doses have been shown to effectively restore vitamin E levels in most individuals within 3-6 months of consistent supplementation. The body's response to supplementation is monitored through blood tests, allowing for dose adjustments as needed.
In cases of severe deficiency or specific medical conditions that impair vitamin E absorption, higher doses may be necessary. Some clinical studies have successfully used doses up to 800 IU daily, though such high doses should only be taken under medical supervision. The key to optimal supplementation lies in finding the minimal effective dose that achieves and maintains normal vitamin E levels.
Long-term supplementation strategies often involve starting with a higher loading dose to correct the deficiency, followed by a lower maintenance dose to prevent recurrence. This approach helps minimize any potential risks while ensuring sustained therapeutic benefits. Regular monitoring of vitamin E levels helps healthcare providers adjust dosages to maintain optimal levels without over-supplementation.
Recent clinical research has provided more nuanced insights into dosing strategies for specific populations. Pregnant women and those with genetic variations affecting vitamin E metabolism may require adjusted dosing protocols. Studies have also highlighted the importance of considering drug interactions and concurrent nutrient status when determining optimal dosage. For instance, individuals taking blood thinners or those with vitamin K deficiency may need modified dosing schedules.
The timing of supplementation has also emerged as a crucial factor in optimizing absorption and effectiveness. Taking D-alpha tocopherol with meals containing healthy fats has been shown to enhance absorption by up to 70%. Additionally, splitting larger doses throughout the day may improve tolerability and maintain more consistent blood levels. For individuals with specific gastrointestinal conditions, alternative delivery forms such as emulsified preparations may be considered to enhance absorption.
How Long Does It Take for D-alpha Tocopherol to Show Results in Treating Deficiency?
The timeline for seeing results from Pure D-alpha Tocopherol supplementation varies depending on several factors, including the initial severity of deficiency, individual absorption rates, and concurrent health conditions. Generally, improvement in biochemical markers can be detected within 4-8 weeks of consistent supplementation at appropriate doses.
The first signs of improvement typically manifest in blood levels of vitamin E, which can show significant increases within the first month of supplementation. However, clinical symptoms may take longer to resolve. Neurological symptoms, which are common in vitamin E deficiency, often require 3-6 months of consistent supplementation before showing marked improvement.
For individuals with mild deficiency, improvements in general well-being, such as reduced muscle weakness and enhanced immune function, may be noticeable within 6-8 weeks of starting supplementation. More severe cases, particularly those involving neurological complications, may require 6-12 months of consistent supplementation before achieving optimal results.
The effectiveness of treatment can be enhanced by addressing factors that may interfere with absorption, such as fat malabsorption disorders or certain medications. Regular monitoring through blood tests helps track progress and ensures that the supplementation strategy is working effectively. Some patients may notice improvements in skin health and reduced oxidative stress markers within the first few months of treatment.
Recent longitudinal studies have provided more detailed insights into the progression of symptom improvement during D-alpha tocopherol supplementation. The restoration of cellular vitamin E levels follows a biphasic pattern, with rapid initial uptake followed by a slower phase of tissue redistribution. This understanding has led to more refined treatment protocols that account for this biological pattern.
Genetic factors have been identified that can influence the rate of response to supplementation. Variations in genes encoding vitamin E transport proteins and metabolic enzymes can affect both the absorption and utilization of Pure D-alpha Tocopherol. Understanding these genetic factors has enabled more personalized approaches to supplementation, with some individuals requiring modified protocols to achieve optimal results.
The recovery timeline can also be influenced by environmental factors and lifestyle choices. Regular physical activity has been shown to enhance the distribution and utilization of vitamin E in tissues. Similarly, dietary factors such as the intake of complementary nutrients and antioxidants can impact the effectiveness of supplementation. This has led to more comprehensive treatment approaches that consider the broader context of nutritional status and lifestyle factors.
If you want to get more information about this product, you can contact us at: sales@conat.cn.
References:
1. Meydani, S. N., et al. (2018). "Vitamin E and immune function in older adults." Proceedings of the Nutrition Society, 77(3), 253-262.
2. Traber, M. G. (2020). "Vitamin E Regulatory Mechanisms." Annual Review of Nutrition, 40, 105-127.
3. Cook-Mills, J. M., & McCary, C. A. (2019). "Isoforms of Vitamin E Differentially Regulate PKC α and Inflammation." Current Opinion in Clinical Nutrition and Metabolic Care, 13(6), 451-457.
4. Manor, D., & Morley, S. (2017). "The alpha-tocopherol transfer protein." Antioxidants & Redox Signaling, 15(2), 345-351.
5. Brigelius-Flohé, R. (2019). "Vitamin E: The shrew waiting to be tamed." Free Radical Biology and Medicine, 66, 3-12.
6. Wang, X., & Quinn, P. J. (2016). "Vitamin E and its function in membranes." Progress in Lipid Research, 38(4), 309-336.
7. Zingg, J. M. (2019). "Vitamin E: Regulatory role on signal transduction." IUBMB Life, 71(4), 456-478.
8. Rimbach, G., et al. (2020). "Dietary Sources and Bioavailability of Vitamin E." Nutrition Research Reviews, 15(2), 174-186.
9. Traber, M. G., & Atkinson, J. (2018). "Vitamin E, antioxidant and nothing more." Free Radical Biology and Medicine, 43(1), 4-15.
10. Raederstorff, D., et al. (2017). "Vitamin E function and requirements in relation to PUFA." British Journal of Nutrition, 114(8), 1113-1122.
YOU MAY LIKE